Days in the dark: For migraine sufferers, recent drug research could afford bearable light at the end of the tunnel
Migraine is ranked by the World Health Organization (WHO) as the seventh most disabling disease and the leading cause of disability among all neurological disorders.
Such is the severity of migraine in its harshest manifestation that the august body considers it to be as debilitating as quadriplegia, according to Dr Mark Weatherall, Consultant Neurologist at the Buckinghamshire Healthcare NHS Trust in the UK.
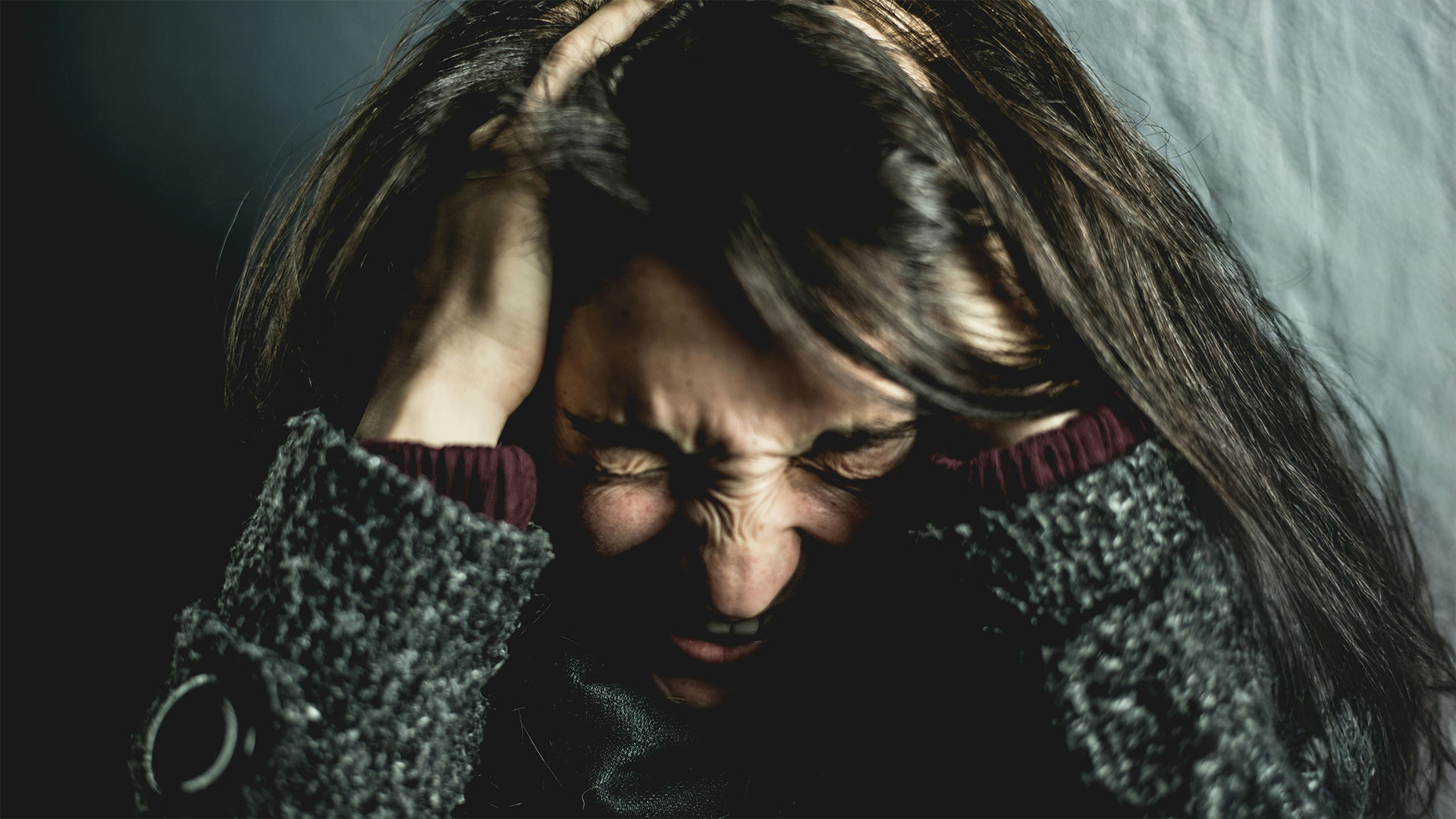
“Now that sounds ridiculous on one level, but it is not really,” he says in a BBC podcast. “Because if you think about someone in the throes of a severe migraine attack, they are bedbound, they are vomiting, they can’t move, they can’t bear the light, they can’t bear the noise. They cannot do anything.”
Widespread suffering
Up to one billion people in the world are believed to suffer from migraine. The onset and causes of the disorder are thought to vary from person to person and the symptoms, likewise, differ considerably. A migraine may last for just a few minutes or as long as a few days, though several hours is often cited as common. Major symptoms include a throbbing head, nausea, dizziness and disturbed vision, yet any of the human senses can be affected, from phantom smells to tingling skin.

Though conceding it is not a permanent disability, the headache specialist notes that the lives of people who have migraine daily or almost every day will be severely impacted. Carrying out normal routine activities or holding down a job may not be possible. Ultimately, acute migraine can wreck lives. Some sufferers have said they become emotionally withdrawn from family and friends.
Until relatively recently, the condition has been little understood. It was not widely studied in the medical community, resulting in misdiagnosis. For instance, those struggling to find the right words for things during a migraine attack have been rushed to hospital with doctors suspecting stroke or a brain tumour.
Hallucinatory hell
Visual disturbance comes under a range of symptoms called the migraine aura, which occurs in about 20-30% of sufferers. Relating to the focal area of dysfunction in the brain, auras can be flashing lights, wavy lines or a much more complex hallucinatory experience. The latter can be terrifying for the migraineur in the first unknowing instances – that is, before the extent and intensity of the sensations have been fully explained to the sufferer.
During an aura, some people feel an overwhelming sense of fatigue and have reported seeing hexagonal shapes as if they were looking through the eye of a fly. A simpler visual disturbance is photopsia, which consists of circles, triangles, squares and other geometric patterns, usually white or multicoloured.

Although these can be seen in any part of the migraineur’s visual field, it is actually a trick of the perceptual imagination; the patterns and shapes are not there in reality. Their occurrence is most likely unrelated to the eye itself and caused by irritation of the vision centre of the brain. More complex and symmetrical patterns can sometimes be seen, and even the blind have been known to experience this disturbing phenomenon.
Distorted perception
Some disturbances are so bizarre that patients delay seeing a doctor for fear of being thought mentally ill. Objects can appear distorted and contorted in some types of visual aura, as if being visualised through a funhouse mirror; body proportions seem out of shape, necks become larger and legs look abnormally small. This is aptly called Alice in Wonderland syndrome since author Lewis Carroll was afflicted by migraine and used his bizarre hallucinatory attacks as inspiration to create Alice and her magical world.
Changes in distance perceptions are also a feature of visual aura – how close or far away objects seem to the beholder could be totally unrelated to reality.
Distortions of sensation or movement are characteristics of classic aura. Tingles or numbness on one side of the face and in the hands and arms can become alarming very quickly. Weakness and clumsiness can occur, while dizziness or abnormal sensations of motion or auditory misperceptions such as a ringing or crackling noise in the ears have been reported. For some sufferers, irritation in the part of the brain that handles memory also results in amnesia.
Pulsating headaches
Migraine headaches are divided into two subtypes – classic migraine which has the aforementioned aura, and common migraine which appears with no aura. They usually affect the frontal forehead region as well as the eyes – an initial pressing, gripping pain that later progresses to a throbbing, banging, pounding headache.

While headaches can be absent altogether (silent migraine), in some cases they are agonisingly painful, affecting the person’s entire skull; their ferocious intensity can entice suicidal thoughts. The scalp can become very tender during a severe migraine attack and sneezing, coughing and vomiting can become extremely painful.
People with a prolonged history of migraine headaches should seek professional support if their headaches do not fit a recognisable pattern, or when abnormal physical symptoms are apparent.
Triggers of attack
The exact cause of migraine is not clear, although spinal disorders, hormonal fluctuations, stress, fatigue, sleepless nights, certain odours, allergic reactions, glaring sunlight, diet, caffeine, exercise, levels of hydration, cigarette smoke and smoking itself have all been cited as contributory factors. Some people have even reported experiencing migraine headaches during sexual activity, especially at the moment of orgasm. For others, barometric pressure or altitude changes are believed to have triggered attacks. Avoidance of triggers may help, but attacks will usually still occur.

Constriction of blood vessels was once theorised as a cause, but it is now thought that nerves in the body drive migraines. Weatherall notes that normal processes in the body dealing with sensory input go awry during a migraine attack. “You start to get signals sent out to the blood vessels around the head and the neck, and various neurochemicals are released. The lynchpin molecule, calcitonin gene-related peptide, is picked up by receptors around the blood vessels, which starts to generate pain. As that process continues, other networks start to become engaged that may make us feel nauseous or sensitive to light or noise,” he explains.
Effective drugs
Medical research conducted into ways to block or ease the transmission of overactive pain nerves has highlighted a relationship between serotonin, a chemical messenger in the brain, and migraine. The triptan family of drugs has demonstrated efficacy in halting migraine attacks by affecting serotonin receptors. These drugs are often prescribed to patients when other preventative medications, such as painkillers or beta blockers, fail to provide relief. By imitating the actions of serotonin, these drugs ease overactive pain nerves
A major new study led by the University of Oxford and involving more than 89,000 people has found that triptans are the most effective medicine for adults experiencing acute migraine. It compared the effectiveness of 17 different oral medications often used to treat the condition. The results were published in The British Medical Journal this summer.







