
Ill Feeling: Hypochondria is a living hell for those whose profound fears about their health cannot be relieved
Anxiety, an increasing concern in recent years particularly among young people, is detrimental to health, but what if it is excessive worry about your health that troubles you? Exaggerated feelings of unease about having or developing a serious undiagnosed medical condition are nothing new. The Greek physician Hippocrates first used the word hypochondria in the fifth century BCE, and it has been the subject of discussion and study through every era since, with a vast and bewildering literature dedicated to the subject.
Around the 17th century, hypochondria had come to denote a mysterious and melancholy condition thought to result in an imbalance in the organs of the abdomen; then gradually, it was used to refer to any illness without a detectable cause. It is generally considered shorthand for an illness that is all in your head.

Hypochondriasis is a psychiatric disorder with very specific diagnostic criteria. Health anxiety is a much broader term used today to describe such conditions, which can encompass depression, various anxiety disorders, chronic illness and pain, among other problems.
A diagnosis of hypochondriasis or illness anxiety disorder usually entails the following: a preoccupation with a fear of having a serious disease based on misinterpreting the meaning of physical symptoms, which persists despite medical tests showing nothing is wrong and reassurance from doctors, is present for at least six months, and is not focused exclusively on a concern about physical appearance; and an awareness on some level that this fear may not be 100% accurate.
Personal battle
British writer Caroline Crampton lives in constant fear that there is something seriously wrong with her. In a moving and heartrending story of a hypochondriac in the throes of despair, she details her personal battle with the debilitating condition.
It all began when she was 17 and developed blood cancer, which was only discovered after a tumour had appeared on her neck. Following several gruelling rounds of chemotherapy, she was given the all-clear, but even though she was cured, she became ever-alert to potential new symptoms, constantly worrying that the cancer may have returned. “The fear that there is something wrong with me, that I am sick, is always with me,” she says in a BBC podcast of her memoirs called A Body Made of Glass.
She tells of a bus journey “half listening to somebody else’s phone call, when I suddenly went deaf”. Her heart beat faster and faster as the fear grew stronger, and her vision blurred into “a sparkling circle of refracted rays”. This sudden loss of hearing and sight happened three more times that week. “There was no pattern to it. I saw a nutritionist, a neurologist, a urologist, a cardiologist, a psychiatrist and an endocrinologist,” she shares.
Contradictory fears
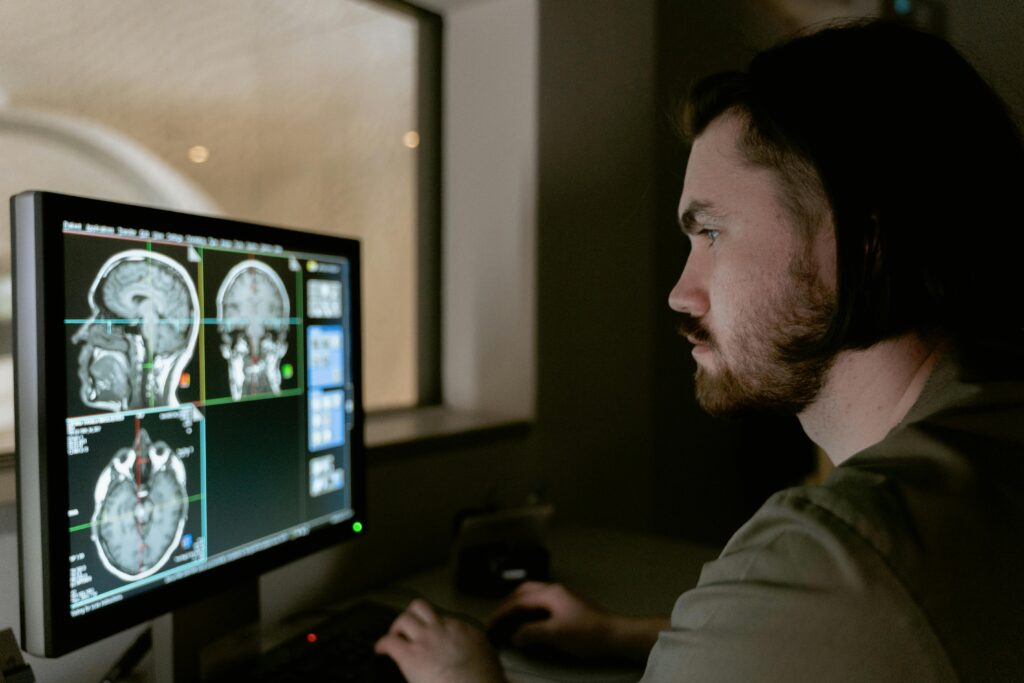
None of her tests showed anything unusual, so she had an MRI. As she lay motionless in the machine, she oscillated between two contradictory hopes: “I really wanted the scan to find something, so that I would have a name to put to my symptoms, and I was terrified that it would deliver the devastating news that I had some life-altering illness.”
Another disturbing thought niggled at her, could she even be satisfied with the results, or would her impulse toward hypochondria convince her that there was something else lurking unseen just out of reach?
The scan revealed nothing of concern, and this was the end of the road diagnostically. The answer to the baffling question of her hearing and vision problems was never discovered. She was given a small daily dose of a medication for low blood pressure, which reduced the number of episodes from several a week to just a few a year. “I still take this pill every day, dutifully refilling the prescription every month, despite having no idea why I am doing so or what malfunction of my body it is treating,” she says.
Nothing is wrong
Crampton has lost count of the number of times that she has been to the doctor only to be told the best thing to do is nothing at all. “This is hard advice to receive; the human craving for satisfying narrative demands an explanation for our suffering. Do something it screams – make an appointment, swallow a pill, take a test.”
It took her a long time to entertain the idea that she might be a hypochondriac. It was much easier for her to see in hindsight. She had been encouraged by doctors to pay close attention to how she was feeling, in case she could pick up on an early warning sign of recurrence of her cancer.
Following her all-clear, she gradually came to realise that her level of interest in her fluctuating state of wellness was far from the norm. The sheer variety of procedures she had undergone had given her a level of comfort with the rarer elements of medicine that was unusual.
Good at being unwell
“More than that though, the awareness crept up on me that I spent much more time and effort on this aspect of life than anyone else I knew, even though I supposedly had no active conditions requiring treatment. At some point, my responsible cancer survivor behaviour had morphed into something else. Rather than worrying about actual developments with my illness, the worry itself had become the problem,” she reveals.
“And it feels at times like having cancer for real was the training I went through so I could have a dozen other illnesses in my imagination. I am now very good at being unwell. I have had a lot of practice.”
She believes most people have some legitimate concern about at least one aspect of their health, whether it is a prior condition, a family history or an environmental factor. “Hypochondria creeps in when this justifiable anxiety expands well beyond the boundaries of the verifiable health concern. For example, when someone with a chronic back injury becomes convinced that they have mouth cancer.”
Safety and avoidance
People with elevated levels of health anxiety are known to rely on safety behaviours or often avoid feared situations. Safety behaviours may include seeking reassurance from family and friends, doctors, medical books or the Internet; requesting frequent unnecessary medical tests; and monitoring physical symptoms, such as pain, racing heart, dizziness or blurred vision.

Alternatively, some people with a form of health anxiety avoid feared stimuli, which keeps their fear alive over the longer term. They may put off medical tests or seeing a doctor, or talking to others about health, illness or a feared disease. Experts suggest these strategies are counterproductive and advise confronting feared situations directly, and accepting feelings of anxiety and fear rather than trying to control them.
Symptom management
There are no straightforward answers to this chronic mental illness. Cognitive behavioural therapy, stress management and mindfulness techniques, such as meditation, may help manage symptoms.
The impact of the Covid pandemic has lifted already rising rates of hypochondria, and a study in Norway has shown that high levels of anxiety about one’s own health can increase the risk of heart disease by up to 70%. As Crampton observes: “It would seem that worrying about being ill can, in fact, make you ill.”







